Abstract
Background
Nodular lymphocyte-predominant Hodgkin lymphoma (NLPHL) is a rare subtype of Hodgkin lymphoma that typically presents with early-stage favorable disease and exhibits an indolent clinical course with long-term remissions and eventual relapse. Histopathologic variants of NLPHL have recently been described and may have poorer outcomes compared to typical NLPHL. Risk of transformation of variant NLPHL has not been previously described.
Methods
We retrieved patients with NLPHL diagnosed between 2001 and 2016 whose cases had been reviewed at the University of Chicago and who had available clinical information. Patient characteristics, initial histology, treatment history, history of progression and histologically-verified transformation, and survival status were obtained from the electronic medical record. Patients were grouped into three cohorts: NLPHL, variant NLPHL, and transformed NLPHL (t-NLPHL) at diagnosis. t-NLPHL included diffuse large B-cell lymphoma (t-NLPHL/DLBCL) and T-cell/histiocyte-rich large B-cell lymphoma (t-NLPHL/THRBCL) histologies. Standard descriptive statistical analyses were performed. Relapse-free survival (RFS), transformation-free survival (TFS), and overall survival (OS) were estimated by the Kaplan-Meier method. All statistical analyses were performed using STATA, version 15.1.
Results
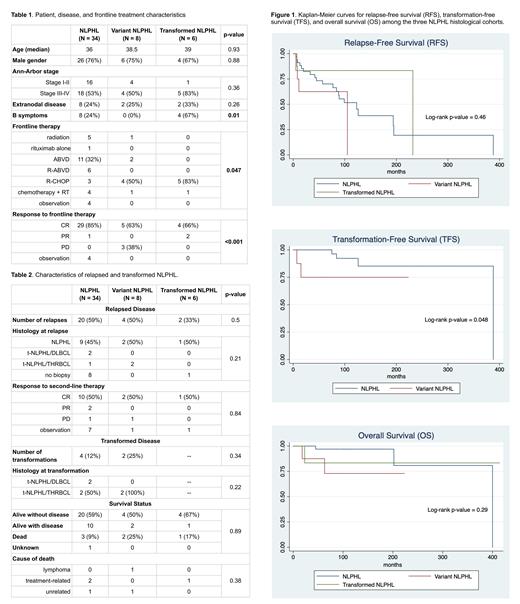
There were 48 patients with newly-diagnosed NLPHL: 34 with NLPHL (71%), 8 with variant NLPHL (17%), and 6 with t-NLPHL (13%) at diagnosis. Patient, disease and frontline treatment characteristics are displayed in Table 1. There was no significant difference in age, male predominance, initial disease stage, or presence of extranodal disease between the three cohorts. B symptoms were more likely in t-NLPHL, and patients with t-NLPHL at diagnosis were more likely to receive frontline R-CHOP. Patients with variant NLPHL were significantly more likely to have progressive disease after frontline therapy.
A total of 26 patients (54%) developed relapsed disease and 6 (13%) developed subsequent t-NLPHL (Table 2). The majority of histologically-confirmed relapses were NLPHL (N = 12, 71%), and the majority of subsequent transformations were t-NLPHL/THRBCL (N = 4, 66%). Nearly all of the patients with subsequent transformations developed t-NLPHL at the time of first relapse (N = 5, 83%). There was no significant difference in incidence of relapse or histology at relapse, nor was there any difference in incidence of transformation or histology at transformation, between the three cohorts.
RFS, TFS and OS for each cohort are displayed in Figure 1, with a median follow-up of 8.5 years (range 1.5-34.5 years). Between the three cohorts, there was no significant difference in RFS (p = 0.46) or OS (p = 0.29). There was a significant difference in TFS between the typical and variant NLPHL cohorts (p = 0.048), although the number of transformation events was low. A total of 6 patients (13%) died, with no significant difference in incidence of death or cause of death between the three cohorts (Table 2). Only 1 patient in the entire cohort died from lymphoma, a patient with variant NLPHL who died of transformed lymphoma. There were three deaths secondary to treatment (myelodysplastic syndrome, acute lymphocytic leukemia, and cardiomyopathy).
Conclusions
This single-center retrospective study suggests that variant NLPHL was less likely to respond to frontline therapy and had a shorter transformation-free survival compared to typical NLPHL, but without compromise in terms of PFS and OS. This suggests that current salvage therapies are effective for relapsed and transformed variant NLPHL. Investigation of transformation risk in variant NLPHL with larger datasets is warranted.
Smith: Alexion, AstraZeneca Rare Disease: Other: Study investigator; Celgene, Genetech, AbbVie: Consultancy. Venkataraman: EUSA Pharma: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal